The shoulder is the most mobile joint in the body. It allows one to lift the arm, rotate it, and reach up overhead. It is able to turn in many directions. This greater range of motion, however, results in less stability.
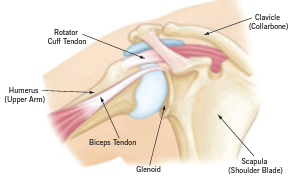
The shoulder is made up of three bones: humerus (upper arm bone), scapula (shoulder blade), and clavicle (collarbone). Shoulder dislocations can be partial, with the ball of the upper arm coming just partially out of the socket. This is called a subluxation. A complete dislocation means the ball comes all the way out of the socket.
How do shoulder dislocations happen?
Shoulder instability occurs when the head of humerus (the upper arm bone) is forced out of the shoulder socket. This usually occurs as a result of a sudden traumatic injury.
Once a shoulder has dislocated, it is vulnerable to repeat episodes. When the shoulder is loose and slips out of place repeatedly, it is called chronic shoulder instability.
What are the symptoms of shoulder instability?
Common symptoms of chronic shoulder instability include:
- Pain caused by shoulder injury
- Repeated shoulder dislocations
- Repeated instances of the shoulder giving out
- A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just “hanging there”
How is shoulder instability diagnosed?
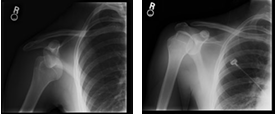
There are specific tests that help assess instability in the shoulder, including general looseness in ligaments. A doctor may order imaging tests, including X‑rays, CT scan, or MRI to help confirm a diagnosis and identify any other problems.
How is shoulder instability treated and how long is recovery?
Chronic shoulder instability is often first treated with nonsurgical options. If these options do not relieve the pain and instability, surgery may be needed.
Nonsurgical Treatment
It often takes several months of nonsurgical treatment before an assessment of success can be made. Nonsurgical treatment typically includes:
- Activity modification
- Non-steroidal anti-inflammatory medication
- Physical therapy
Surgical Treatment
Surgery is often necessary to repair torn or stretched ligaments so that they are better able to hold the shoulder joint in place.
- Bankhart lesions (tearing of the front labrum from the socket) can be surgically repaired by using suture anchors to reattach the ligament to the bone.
- Arthroscopy—Soft tissues in the shoulder can be repaired using tiny instruments and small incisions. This is a sameday or outpatient procedure. Arthroscopy is minimally invasive surgery. A surgeon will look inside the shoulder with a tiny camera and perform the surgery with special instruments.
- Open Surgery—Some patients may need an open surgical procedure. This involves making a larger incision over the shoulder and performing the repair under direct visualization.
Rehabilitation
After surgery, the shoulder may be immobilized temporarily with a sling. When the sling is removed, exercises to rehabilitate the ligaments will be started. These will improve the range of motion in the shoulder and prevent scarring as the ligaments heal. Exercises to strengthen a shoulder will gradually be added to a rehabilitation plan.
Source:
https://www.sportsmed.org/aossmimis/STOP/Prevent_Injuries/Revised/Injury/Shoulder%20Instability.pdf
